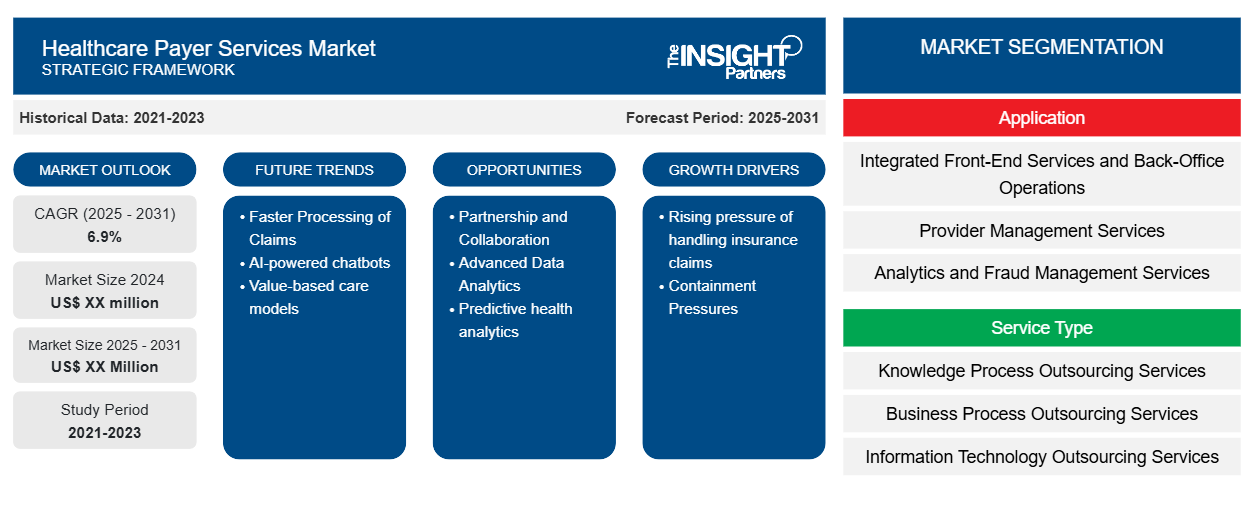
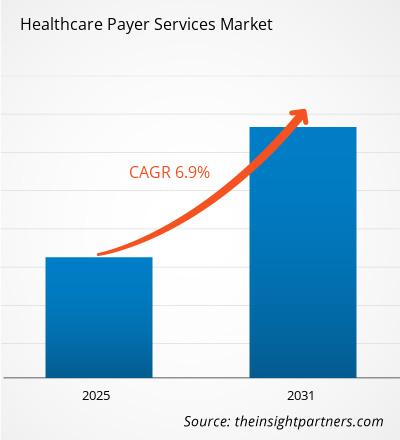
The Healthcare Payer Services Market is expected to register a CAGR of 6.9% from 2025 to 2031, with a market size expanding from US$ XX million in 2024 to US$ XX Million by 2031.
The Healthcare Payer Services Market report offers a comprehensive analysis segmented into key categories, including Service Type, Application, End User and Geography. It features a regional breakdown, highlighting significant markets and countries to provide a global perspective. Market evaluations are expressed in US dollars (US$), facilitating a nuanced understanding of market dynamics, growth trends, and competitive landscapes across various regions and segments. This insight enables stakeholders to identify opportunities and make informed decisions within the rapidly evolving landscape of healthcare payer services.
Purpose of the Report
The report Healthcare Payer Services Market by The Insight Partners aims to describe the present landscape and future growth, top driving factors, challenges, and opportunities. This will provide insights to various business stakeholders, such as:
- Technology Providers/Manufacturers: To understand the evolving market dynamics and know the potential growth opportunities, enabling them to make informed strategic decisions.
- Investors: To conduct a comprehensive trend analysis regarding the market growth rate, market financial projections, and opportunities that exist across the value chain.
- Regulatory bodies: To regulate policies and police activities in the market with the aim of minimizing abuse, preserving investor trust and confidence, and upholding the integrity and stability of the market.
Healthcare Payer Services Market Segmentation
Application
- Integrated Front-End Services and Back-Office Operations
- Provider Management Services
- Analytics and Fraud Management Services
- Billing and Accounts Management Services
- HR Services
- Claims Management Services
Service Type
- Knowledge Process Outsourcing Services
- Business Process Outsourcing Services
- Information Technology Outsourcing Services
End User
- Public Players
- Private Players
Geography
- North America
- Europe
- Asia-Pacific
- South and Central America
- Middle East and Africa
Customize This Report To Suit Your Requirement
You will get customization on any report - free of charge - including parts of this report, or country-level analysis, Excel Data pack, as well as avail great offers and discounts for start-ups & universities
Healthcare Payer Services Market: Strategic Insights
- Get Top Key Market Trends of this report.This FREE sample will include data analysis, ranging from market trends to estimates and forecasts.
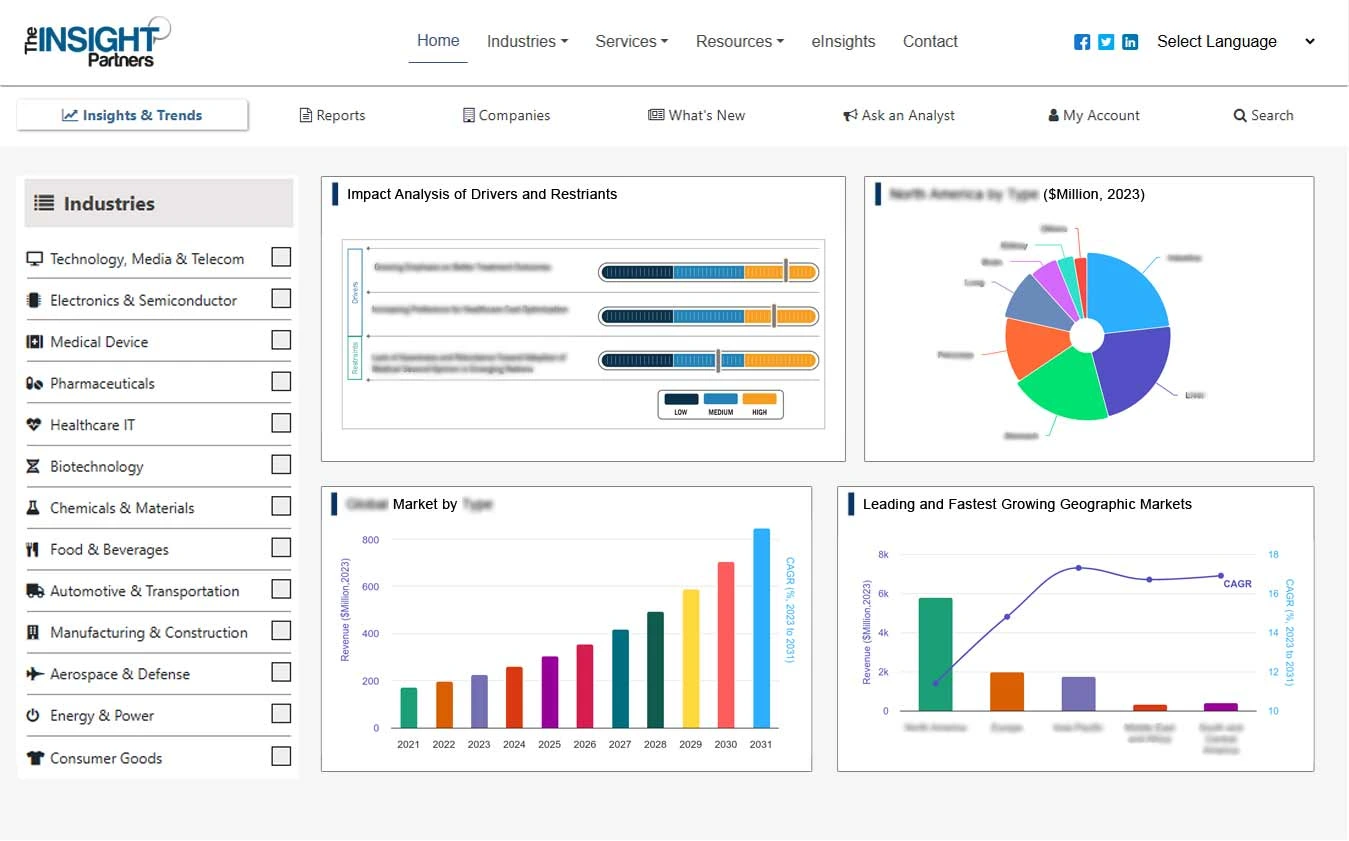
Healthcare Payer Services Market Growth Drivers
- Rising pressure of handling insurance claims: health insurance sectors have been developing rapidly, the healthcare payer services market size is expanding due to rising pressure for handling an additional number of members thus driving demand for this market. share in the global healthcare payers services market
- The Need for Control over Expenses: There is an emerging need for healthcare payers to control their operating and administrative expenses without compromising the high quality of care. According to a recent Commonwealth Fund research, 8-10% of US healthcare spending is thought to be attributable to administrative costs.
- Containment Pressures: Increased pressure to manage both administrative and operational costs while continuing to provide service at the highest levels, healthpayers are seeking strategies that will save them costs. As estimated by commonwealth funds the administrative costs make up about 8-10% of health expenditures in the U.S. Payers outsource more of the non-core functions. These non-core functions include claims management, customer service, and enrollment processing, to specialist vendors in a bid to save on costs. This healthcare payer services market forecast indicates, that outsourced payer services enable organizations to achieve operational efficiencies, enhance service quality, and focus more intently on core strategic initiatives such as policy development and member engagement, leading to significant market growth.
Healthcare Payer Services Market Future Trends
- Faster Processing of Claims: payers should be able to process large volumes of claims not only much faster but with fewer errors. According to a report by Accenture, AI could cut as much as $150 billion in annual healthcare administrative manageables in the US by 2026.
- AI-powered chatbots: AI chatboats in customer service provide immediate support for inquiries about benefits, status of claims, and general policy inquiries.
- Value-based care models: Moving away from fee-for-service models to the focus of value-based care means payers will need to attach reimbursement to patient outcomes, not to volume. The shift to value-based care requires rethinking how the operations of provider networks are handled, analysis of patient data, and rewards for taking preventive measures. Payer concerns around care coordination and population health management are only getting worse as the sector increasingly shifts toward value-based care. For ensuring that providers meet the quality requirements, analytics and prediction models provide much-required insight into patient outcomes. In this respect, the frontrunners are Medicare and Medicaid. A general belief has emerged that by mid-decade, most reimbursements will be value-based, with quality of care the driving force in paying. This is causing a ripple effect, as more and more private payers are following suit.
- Outsourcing non-core functions: Indeed, the future will be bright for outsourcing non-core functions in healthcare as payers start looking at resources as the number one priority while reducing operational costs in non-core functions such as claims processing and customer service. Outsourcing is cost-effective since it allows payers to respond quickly to either regulatory changes or market demands. Recent solutions by third-party payer service providers include AI and cloud-based systems, as well, to further make the process smoother with fewer manual errors.
Healthcare Payer Services Market Opportunities
- Partnership and Collaboration: Payers can collaborate in the design and implementation of integrated care platforms with care providers, pharmaceutical companies, and technology companies to enhance care coordination and improve patient outcomes.
- Advanced Data Analytics: Fraud Detection and Prevention: Various types of healthcare fraud account for billions of dollars annually. In this regard, AI-based fraud detection systems, hence, have turned to be in high demand. Those companies offering fraud detection solutions help the payers by highlighting suspicious claims that minimize risks and save a great amount in the process.
- Predictive health analytics: Payers will be able to anticipate member needs, and optimize pathways of care. Furthermore it will prevent hospital readmissions. Vendors offering analytics platforms, together with AI-driven tools, will see opportunities in supporting payers in the delivery of personalized care plans with improved population health outcomes.
Healthcare Payer Services Market Regional Insights
The regional trends and factors influencing the Healthcare Payer Services Market throughout the forecast period have been thoroughly explained by the analysts at Insight Partners. This section also discusses Healthcare Payer Services Market segments and geography across North America, Europe, Asia Pacific, Middle East and Africa, and South and Central America.
- Get the Regional Specific Data for Healthcare Payer Services Market
Healthcare Payer Services Market Report Scope
| Report Attribute | Details |
|---|---|
| Market size in 2024 | US$ XX million |
| Market Size by 2031 | US$ XX Million |
| Global CAGR (2025 - 2031) | 6.9% |
| Historical Data | 2021-2023 |
| Forecast period | 2025-2031 |
| Segments Covered |
By Application
|
| Regions and Countries Covered | North America
|
| Market leaders and key company profiles |
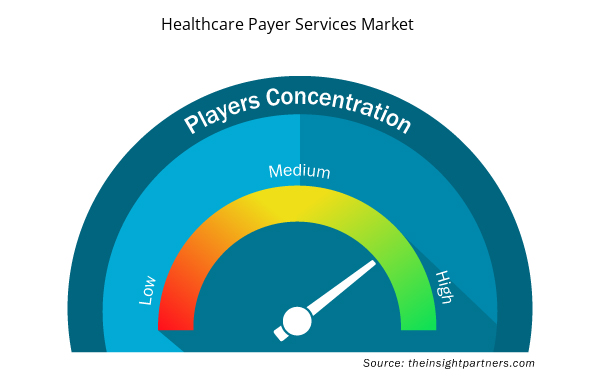
Healthcare Payer Services Market Players Density: Understanding Its Impact on Business Dynamics
The Healthcare Payer Services Market market is growing rapidly, driven by increasing end-user demand due to factors such as evolving consumer preferences, technological advancements, and greater awareness of the product's benefits. As demand rises, businesses are expanding their offerings, innovating to meet consumer needs, and capitalizing on emerging trends, which further fuels market growth.
Market players density refers to the distribution of firms or companies operating within a particular market or industry. It indicates how many competitors (market players) are present in a given market space relative to its size or total market value.
Major Companies operating in the Healthcare Payer Services Market are:
- Cognizant Technology Solutions
- Accenture plc.
- Concentrix Corporation
- ExlService Holdings, Inc.
- Xerox Corporation
Disclaimer: The companies listed above are not ranked in any particular order.
- Get the Healthcare Payer Services Market top key players overview
Key Selling Points
- Comprehensive Coverage: The report comprehensively covers the analysis of products, services, types, and end users of the Healthcare Payer Services Market, providing a holistic landscape.
- Expert Analysis: The report is compiled based on the in-depth understanding of industry experts and analysts.
- Up-to-date Information: The report assures business relevance due to its coverage of recent information and data trends.
- Customization Options: This report can be customized to cater to specific client requirements and suit the business strategies aptly.
The research report on the Healthcare Payer Services Market can, therefore, help spearhead the trail of decoding and understanding the industry scenario and growth prospects. Although there can be a few valid concerns, the overall benefits of this report tend to outweigh the disadvantages.
- Historical Analysis (2 Years), Base Year, Forecast (7 Years) with CAGR
- PEST and SWOT Analysis
- Market Size Value / Volume - Global, Regional, Country
- Industry and Competitive Landscape
- Excel Dataset
- Hair Extensions Market
- Artificial Intelligence in Healthcare Diagnosis Market
- Print Management Software Market
- Aerospace Forging Market
- Single Pair Ethernet Market
- Online Exam Proctoring Market
- Airport Runway FOD Detection Systems Market
- Authentication and Brand Protection Market
- Antibiotics Market
- Aircraft Wire and Cable Market
Report Coverage
Revenue forecast, Company Analysis, Industry landscape, Growth factors, and Trends
Segment Covered
This text is related
to segments covered.
Regional Scope
North America, Europe, Asia Pacific, Middle East & Africa, South & Central America
Country Scope
This text is related
to country scope.
Frequently Asked Questions
Some of the customization options available based on request are additional 3-5 company profiles and country-specific analysis of 3-5 countries of your choice. Customizations are to be requested/discussed before making final order confirmation, as our team would review the same and check the feasibility.
The report can be delivered in PDF/PPT format; we can also share excel dataset based on the request.
The leading players in this market are- Cognizant Technology Solutions, Accenture plc, Concentrix Corporation, ExlService Holdings Inc, Xerox Corporation, Genpact Limited, Hewlett Packard, Hexaware Technologies Limited, FirstSource Solutions Limited.
The market is expected to register a CAGR of 6.9% during 2023-2031
Healthcare payer services market is driven by demographics, regulations, technology, cost control, and outsourcing to improve efficiency and manage expenses.
The market trends include AI integration, value-based care models, analytics for outcomes, and outsourcing non-core functions to enhance efficiency and reduce costs.
Trends and growth analysis reports related to Life Sciences : READ MORE..
1. Cognizant Technology Solutions
2. Accenture plc.
3. Concentrix Corporation
4. ExlService Holdings, Inc.
5. Xerox Corporation
6. Genpact Limited
7. Hewlett-Packard
8. Hexaware Technologies Limited
9. FirstSource Solutions Limited
10. HCL Technologies Ltd.
 Get Free Sample For
Get Free Sample For